Explore our Services
Helping you drive competitive advantage
Discover our global locations
Stay informed. Stay ahead.
Latest whitepaper
Reimagine Customer Experience Management on Social Media
Experience a new world of work
Explore Opportunities
The ResultsCX difference
End-to-end complaints management to boost retention and advocacy
Health plans face significant challenges in complaints management, with unresolved member issues leading to increased churn, lower Star ratings, and strained enrollment and retention efforts. Member complaints arise at various touchpoints in the healthcare journey–ranging from enrollment issues to claims delays, denials, and unsatisfactory settlements–each requiring precise resolution to mitigate risks and maintain compliance.
Backed by decades of expertise, the ResultsCX Complaints Management Program equips health plans to proactively address member concerns and reduce churn. By integrating dedicated complaint management teams with automated workflows and advanced analytics, we identify and resolve issues at an early stage, transforming friction points into opportunities for building loyalty and driving growth.
#ResultsMatter
For timely complaint handling and compliance
1
hr TAT
CTM improvement for a national carrier
1
% YoY
Improvement plans recommended in 2024
1
+ CTM
Maximizing impact across stakeholders
According to the National Association of Insurance Commissioners (NAIC), the top three causes of member complaints are claim handling delays, unsatisfactory settlements, and claim denials. Through comprehensive analysis of complaints data, we detect changing buying patterns and early signs of disenrollment to pinpoint members at risk of churning. These insights enable our frontline teams to engage meaningfully with members and proactively implement targeted interventions to drive retention and long-term success.

CX teams
Proactive identification of potential issues reduces the load on service teams
Members
Hyper personalized and effective resolution improves the member experience
Health plans
Improved member satisfaction and Star ratings lead to increased retention and growth
End-to-end solutions: Boosting efficiency, member satisfaction and Star ratings
While individual issues may seem minor, multiple issues can add up quickly, reaching a tipping point and driving member disenrollment. Our expert complaints taskforce utilizes 7QC tools and complaint call insights to analyze root causes and trends. This allows us to provide targeted recommendations that enhance First Call Resolution (FCR) and Customer Satisfaction (CSAT), while also enabling proactive outreach to address recurring issues throughout the customer journey.
Risk identification
Leverages advanced interaction analytics tools to analyze call data and detect trends before complaints arise, preemptively uncovering potential causes of complaints.
CTM prevention
Harnesses predictive data to drive proactive outreach and intervention, addressing member concerns before they escalate to the CMS’s Complaints Tracking Module (CTM).
Omnichannel outreach
Engages members– across channels–based on a point-based system that highlights the seriousness of complaint, enabling proactive risk management for issues like benefit changes.
Highly skilled advocates
Experienced advocates skilled in complaint resolution and plan advisement use advanced tools to manage member interactions and ensure smooth program launches. Dynamic coaching strengthens follow-ups and processes for higher FCR and improved CSAT.
Operational excellence
Drives operational excellence through accuracy, Root Cause Analysis (RCA), and timeliness–while powering continuous process improvements with actionable insights into people, processes, and systems.

Tech-enhanced, human-centered resolution
By seamlessly blending advanced technology with human expertise, our complaint resolution framework delivers better outcomes–all while preserving the element of empathy essential to successful complaint resolution. We optimize complaint handling through smart classification, triaging, and automated routing, ensuring most cases are resolved at the first point of contact or assigned accurately to either early resolution or specialist teams. Automated business rules evolve continuously to enhance speed, accuracy, and efficiency, ensuring a seamless, customer-focused complaint resolution experience.
- Real time-voice and text analytics
- AI-driven algorithms, knowledge base, and bots
- Personalized adaptive learning
Intelligent root cause analysis
Our tech-driven RCA workflow transforms complaints into powerful insights, driving meaningful improvements in products, services, and processes.
Real-Time Data Capture & Integration
An automated workflow aggregates data from call transcripts, CRM, email, chat, and complaint systems, ensuring a comprehensive, real-time view of the customer journey.
AI-Powered Root Cause Identification
Using Natural Language Processing (NLP), our RCA engine pinpoints complaint drivers and links them to key external factors such as product specs, pricing changes, sales processes, and contact center performance.
Targeted, Actionable Recommendations
Deep insights fuel tangible improvements—whether it’s updating product literature, enhancing training for relationship managers, or refining underwriting checks to prevent recurring issues.
Complaints training, global retail bank
Visual dashboards deliver findings, outlining complaint trends, root causes, and strategic action points to drive long-term improvements.
Skilled and empowered complaints taskforce
By blending targeted coaching with rigorous governance, our Complaints Management Program equips healthcare advocates with the skills and insights needed to effectively resolve member concerns, in turn boosting member experience and loyalty.
Specialized Taskforce Training
Advocates are trained to navigate complex complaint scenarios, ensuring effective resolution and provider education.
Plan Design Expertise
Given the intricacies of plan structures, our team helps health plans communicate plan details more effectively to members.
Root Cause Analysis & Strategic Guidance
The CMT team identifies patterns of dissatisfaction, uncovering underlying issues, guiding plans toward optimal solutions.
Tenured Agents & Advanced Tools
Experienced agents leverage leading-edge tools to manage complaints efficiently and close the loop on member interactions.
Proactive Coaching for Follow-Through
Frontline agents receive targeted coaching on action items like member callbacks, driving process improvements and ensuring speedy resolution.

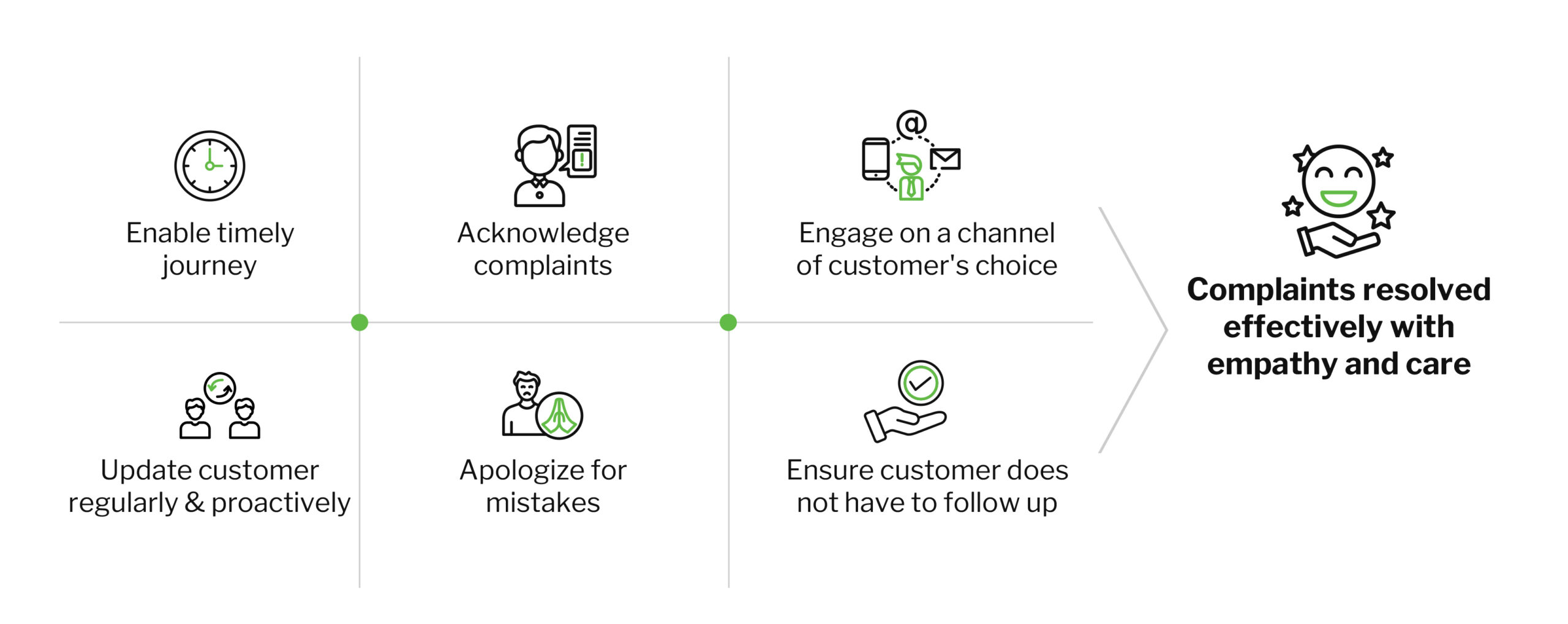
Partner with us: Design a successful complaints journey
With over three decades of complaint management experience, ResultsCX is your trusted partner in designing a seamless and effective complaint handling process. Our flexible resourcing ensures that your operations are equipped to handle varying demands, while our outcome-driven reporting provides clear insights to measure success.
Awards & recognition
We have been recognized a leader across most aspects of our work – from Customer Experience Management (CXM) to security to workplace innovation. We believe that every day brings new opportunities to do better and become better. See what industry analysts and customers are saying about ResultsCX